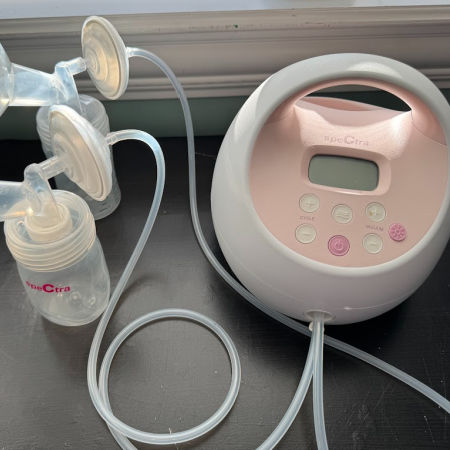
Products We Love
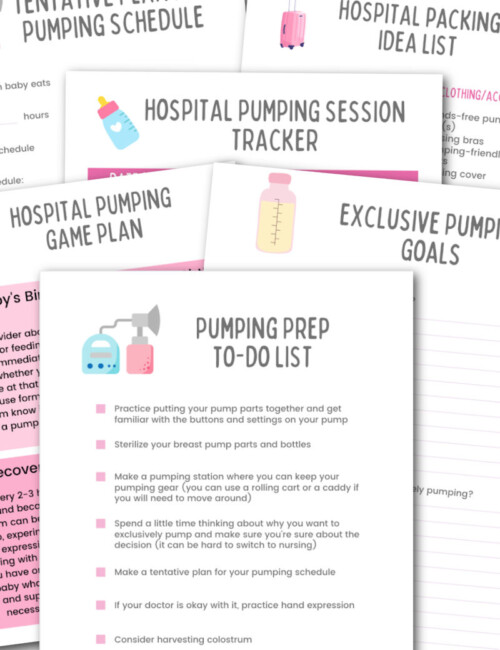
Exclusive Pumping 101
New to exclusively pumping breast milk? Here are all the basics you need to know to be successful.
Increasing Milk Supply
Struggling to pump enough breast milk for your baby? Here are some strategies for increasing pumping output.
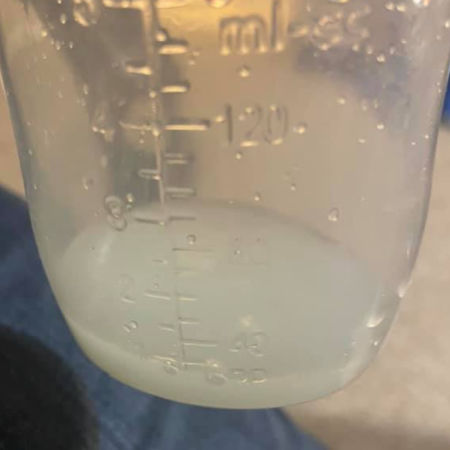
Managing Your Milk and Feeding Your Baby
Here are tips and tricks for breast milk storage as well as bottle feeding your baby breast milk.