If you’re in the US, you may have heard that breast pumps are covered by your health insurance. If you’re pregnant and planning to breastfeed, here’s how to easily get a free breast pump through insurance!
This post may contain affiliate links, which means that if you click through and make a purchase, I’ll be compensated at no additional cost to you. I only recommend products I love! More info here.
How to get a free breast pump through insurance
I thought that getting a breast pump through insurance would be a giant hassle – who wants to deal with the red tape of an insurance company? I almost didn’t even bother.
But it’s actually really easy!
I would recommend skipping dealing with your insurance company altogether and go right to a medical device company that provides breast pumps. Aeroflow Breastpumps is who I recommend.
All you have to do is fill out this form, and they take it from there – they contact your insurance, get the prescription from your doctor, see what you qualify for, and help you pick out a pump.
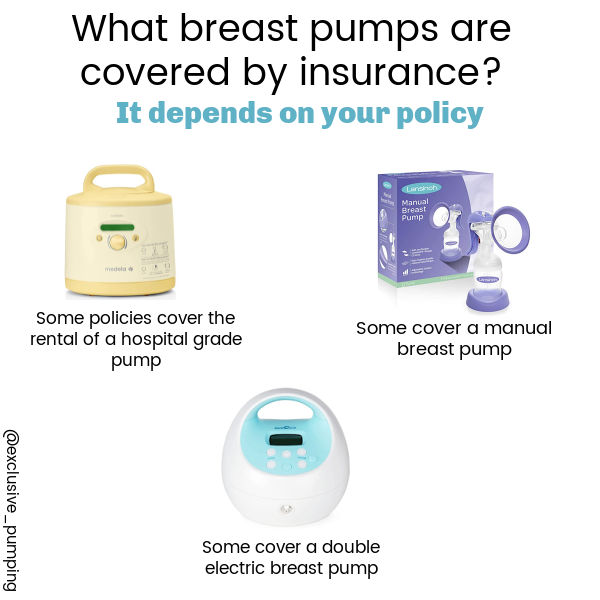
What breast pumps are free through insurance?
It depends on your insurance policy.
Some policies cover rental of a hospital grade pump like the Medela Symphony, others cover a double electric pump like the Spectra S2, and others cover a manual pump like the Lansinoh Manual Breast Pump.
How do you find out which pumps your insurance covers?
After you contact a medical device company that your insurance works with, they will contact your insurance company and find out what breast pumps are covered by your policy.
They will then let you know what your choices are.
Anecdotally speaking, most policies seem to cover a “basic” (but effective) double electric pump. Examples of pumps that are often covered include the Medela Pump in Style with Max Flow, Spectra S2, and Motif Luna.
These breast pumps work great and get the job done, but they don’t always have all the bells and whistles of some more expensive pumps.
What if the pump you want isn’t covered?
In some cases you can upgrade and pay the difference.
For example, if you want a Spectra S1 for the rechargeable battery, but your insurance only covers an S2, you may be able to just pay for the difference in the cost of the two pumps.
Some medical device companies call this an “upgrade option” – just ask the medical device customer service if this is an option for you.
(Breast pump not covered by insurance? Here’s what to do.)
Do you need a prescription to get a breast pump through insurance?
Yes, but in most cases, the medical device company you work with will take care of contacting your health care provider to obtain the prescription for you.
How long does it take to get your breast pump through insurance? When should you get your pump?
It depends on your policy and medical device company.
Some insurance companies will not get you your pump until your baby is born. (Which isn’t ideal for people who plan on exclusively pumping from birth or who end up having a baby in the NICU!)
However, others will provide it within a few weeks of the request, before your baby’s birth.
It may make sense to go ahead and start the process now to ensure that you have the pump when you need it, and aren’t trying to pick a pump when you’re a sleep-deprived parent of a newborn.
What are the breast pump coverage requirements under the Affordable Care Act?
The Health and Human Services department issued the following guidance on what is required by the Affordable Care Act:
Your health insurance plan must cover the cost of a breast pump. It may be either a rental unit or a new one you’ll keep. Your plan may have guidelines on whether the covered pump is manual or electric, the length of the rental, and when you’ll receive it (before or after birth).
The only situation where this rule does not apply is if you have a grandfathered plan.
Grandfathered plans are plans that were in place on March 23, 2010 and have not changed substantially since then. (By now, in 2021, it’s unlikely that you have a grandfathered plan, but it’s still worth checking.) Your insurance company must notify you if you have a grandfathered plan.
The rules do not vary by state, so your insurance company needs to cover a pump regardless of where you live.
Your insurance company is not allowed to charge you a deductible or co-pay for your breast pump.
My experience getting a breast pump from my insurance
With my third baby, I was able to get my own breast pump through insurance when I was eight months pregnant.
As I noted above, it was really easy – I found out on my insurance company’s website which medical device provider they worked with, and went to the website.
After I specified my insurance company and policy number, the medical device company told me which pumps I could choose. I picked a Medela Pump in Style, and placed the order.
After that, I got an email from the company saying they would verify my coverage with my insurance company and my pregnancy with my doctor. And about three weeks after that, my pump arrived.
I didn’t have to speak with anyone on the phone or follow up or anything!
Here’s what I received:

Included was the pump, tubing, two bottles, two sets of pump parts, and some Medela breast pads.
I felt really lucky to get this pump through insurance and have the process be so easy. Because I had already bought a breast pump for my first child, I was able to leave that pump at home and leave this one at work, which made commuting much easier.
Ready to get started? Find out what you qualify for here.
Feel free to share your experience and any tips you have for how to get a breast pump through insurance below!
References- 111th Congress. “Compilation of Patient Protection and Affordable Care Act.” https://housedocs.house.gov/energycommerce/ppacacon.pdf
- Health Resources and Services Administration. “Women’s Preventative Services Guidelines.” https://www.hrsa.gov/womens-guidelines/index.html
- Healthcare.gov. “Breastfeeding Benefits.” https://www.healthcare.gov/coverage/breast-feeding-benefits/
- Healthcare.gov. “Grandfathered health insurance plans.” https://www.healthcare.gov/health-care-law-protections/grandfathered-plans/
- Medela. “Coverage Questions You Should Ask Your Insurance Company.” https://www.medelabreastfeedingus.com/tips-and-solutions/138/coverage-questions-you-should-ask-your-insurance-company
- Medela. “What Does My Insurance Company Cover?” https://www.medelabreastfeedingus.com/tips-and-solutions/166/what-does-my-insurance-company-cover#Infographic














